- Glass skin needs a stable barrier, not intensity.
- Stinging, flushing, or tightness means barrier repair comes first.
- A dermatologist assesses acne, the type of pigmentation, and tolerance before laser treatment.
- Product overload can worsen irritation, acne, and pigmentation.
- Once stable, acne treatment, acne scar treatment, and pigmentation lasers can be sequenced safely.
Why Your Aesthetic Treatment Will Fail: The Truth About “Glass Skin”
In the age of TikTok skincare fads and “instant” laser results, the most critical medical truth is being ignored: you cannot run if you cannot walk.
At DermAlly Singapore, we see a recurring pattern. Patients arrive seeking “Glass Skin” programmes or high-intensity laser treatment to remove pigmentation, yet their skin is already stinging, red, and reactive. They are trying to install a glass roof on a house with a crumbling foundation. When new problems appear, the reflex is to add even more products to solve the growing list of issues.
This is the fundamental difference between aesthetic marketing fads and dermatological science.
If your skin stings, flushes easily, or reacts to basic skincare, book a consult with our team of dermatologists before committing to any laser or peel.
The Real Problem: Consumers Are Used to Self-Diagnosing
The modern consumer journey often starts with a treatment name rather than a diagnosis. Many people discover a procedure on social media, search for it, find a clinic that offers it, and book it. This approach is understandable. Most patients are trying to solve a genuine concern, and online content makes it seem simple to match a problem to a procedure.
The challenge is that skin isn’t straightforward. Online information often highlights best-case results while omitting suitability, risk factors, and aftercare. Without a proper diagnosis, it is easy to choose pico laser Singapore, yellow laser Singapore, or another laser treatment for pigmentation without knowing whether your barrier, inflammation level, or pigmentation type is suitable. Some patients also later discover that the treatment they requested did not target the underlying cause in the first place.
A dermatologist works from a different starting point. Your skin condition determines the plan. The goal is to improve skin health first, then introduce treatments that your skin can tolerate. If a procedure is not suitable because your barrier is compromised, inflammation is active, or pigmentation risk is high, a dermatologist recommends a safer sequence.
It is good to research skincare products, treatments, and ingredients, but to embark on your skin recovery journey, start with a consultation to get a diagnosis-led plan from a dermatologist rather than a treatment-led one informed purely by what you hear online.
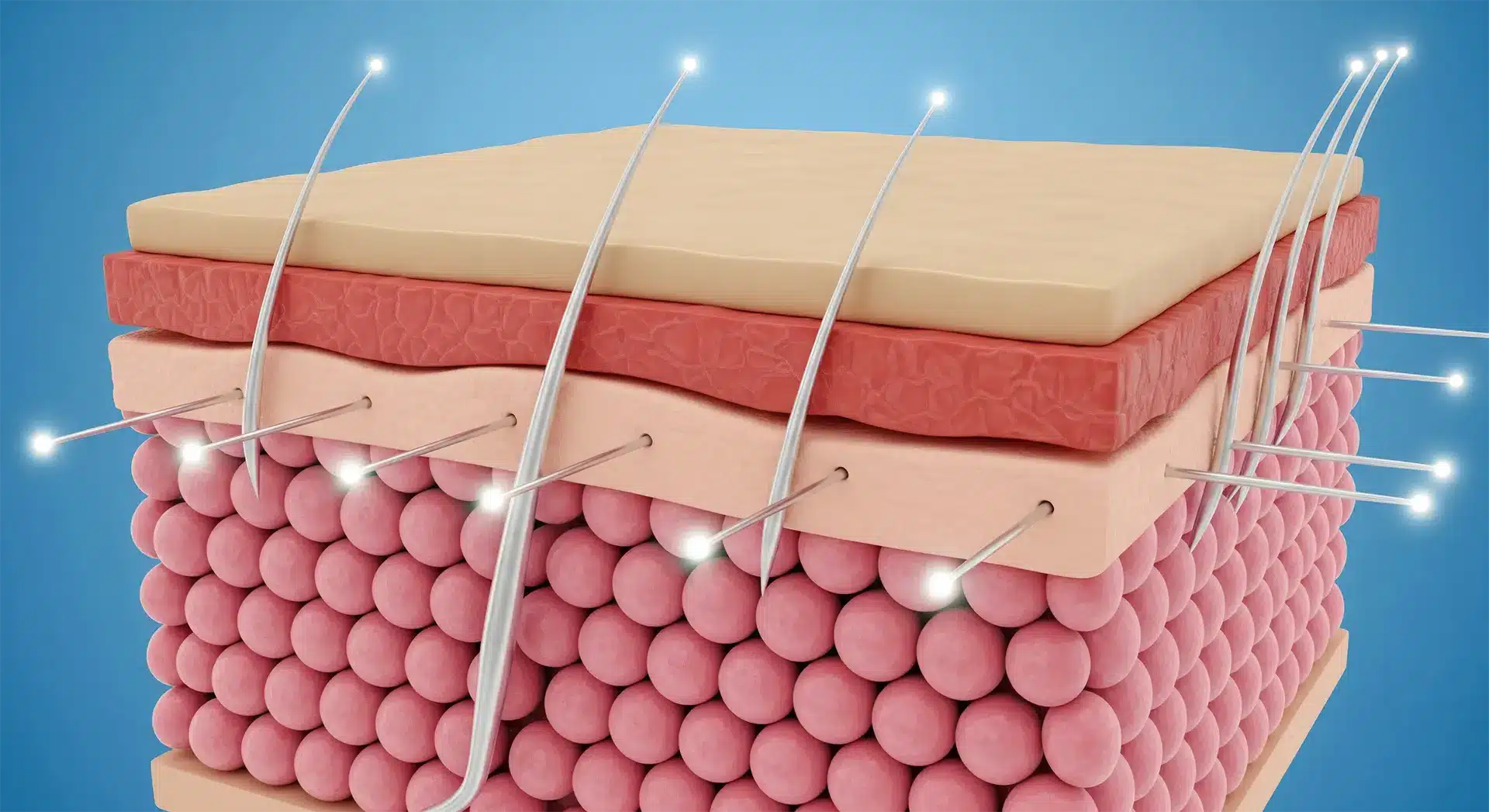
The Skin Barrier Is the Operating System of Your Face
Your skin barrier (mainly the stratum corneum and its lipid matrix) controls hydration, inflammation, and resilience. When it is unstable, everything becomes harder to tolerate, and every treatment carries more risk. This applies to both acne treatment and pigmentation procedures, such as laser for pigmentation removal.
A compromised barrier typically means:
- Higher TEWL (transepidermal water loss): water escapes too quickly, so skin feels tight, rough, and reactive.
- A disrupted acid mantle and pH: the skin’s surface becomes less acidic, which interferes with enzyme activity and increases irritation risk.
- A more fragile immune response: the skin overreacts to “normal” stimuli such as cleansers, sunscreen, or even moisturiser.
If the operating system is crashing, high-performance “apps” like acne laser treatments, deep peels, retinoids, acids, and strong Vitamin C routines frequently trigger inflammation rather than glow.
The First Phase Is Often “De-Prescribing”
Many acne patients do not need more actives. They need fewer triggers.
Social media promotes stacking and “skin cycling” routines. Common combinations include Vitamin C in the morning, retinol at night, AHAs or BHAs several times a week, plus exfoliating toners, masks, and spot treatments. On a weak barrier, this can lead to repeated irritation of inflamed skin. The predictable outcome is burning, peeling, rebound sensitivity, and post-inflammatory marks.
At DermAlly, the first step is often simplification. The goal is to remove products that keep the skin reactive. This is relevant for stubborn breakouts, including hormonal, fungal, and cystic acne.
If you are dealing with persistent breakouts and you have “tried everything”, bring your full skincare routine to our consultation, where we can advise and prescribe based on your personal skin condition.
What “restoring the basics” usually means.
- Reduce irritant load This lowers the daily inflammatory burden, allowing the barrier to rebuild. Common culprits include frequent exfoliation, potent retinoids, acidic toners, harsh foaming cleansers, fragranced actives, and essential oils.
- Rebuild hydration chemistry (NMF support) Natural Moisturising Factors (NMF) are water-binding molecules naturally present in the stratum corneum, which are akin to the skin’s internal “humectant system.” They include compounds such as amino acids and urea that help the skin retain water and remain flexible. When the barrier is damaged, NMF levels drop, TEWL rises, and the skin becomes tight, rough, and easily irritated. Supporting NMF is not about “adding more products.” It is about restoring the skin’s ability to retain water properly.
- Normalise pH (acid mantle stability)
A healthy skin surface is mildly acidic. That acidity matters because it
- helps regulate enzymes responsible for normal shedding (so texture smooths naturally)
- supports barrier lipid organisation
- reduces the risk of microbial overgrowth that can worsen irritation
- Reinforce lipid structure Without the lipid matrix, hydration and NMF cannot function properly because water simply leaks out. This is where barrier repair becomes lipid science, not “moisturising.”
Barrier Repair Is Lipid Science, Not Just “Moisturising”
Barrier repair is not simply applying oil or a thicker cream. The barrier is built from skin-identical lipids arranged in lamellar layers.
The “golden ratio” concept
Barrier lipids are commonly described in a ratio framework:
- Ceramides (structural support)
- Cholesterol (stability and flexibility)
- Free fatty acids (waterproofing and seal)
When this balance is disrupted, the “mortar” between skin cells weakens. The surface becomes leaky and inflamed, and tolerance drops.
MLE Technology: When Formulation Matches Skin Architecture
The barrier is lamellar, meaning it is structured into multiple thin layers. Some formulations are designed to mimic that architecture through Multi-Lamellar Emulsion (MLE) technology, which aims to deliver skin-identical lipids in layered structures that behave more like the skin’s natural lipid matrix.
For compromised skin, the goals are practical:
- patch barrier “gaps” with compatible lipids
- reduce TEWL so hydration stays inside
- support NMF recovery so texture and comfort normalise
- reduce background inflammation so tolerance returns
This is when skin stops feeling “on edge” all the time, and when acne management becomes more stable and less reactive.
Common Misconceptions About Facial Moisturisers vs MLE Moisturisers
Most people misunderstand what a moisturiser is supposed to do, which is why “glass skin” plans often fail before they even begin. These are the most common reasons some moisturisers fail in barrier-impaired acne skin:
Misconception #1: “If it feels rich, it is repairing my barrier”
Many moisturisers feel comforting because they sit on top and reduce water evaporation for a few hours. That is symptom relief, not structural repair.
Barrier repair means restoring the lipid architecture so the skin can hold water on its own. That is where skin-identical lipids and lamellar structure matter. MLE moisturisers aim to mimic the skin’s layered barrier structure, so the product is not just “coating”. It supports barrier rebuilding.
Misconception #2: “Ceramide cream means proper barrier repair”
People see “ceramide” on a label and assume the barrier is covered. Many products include a small amount of ceramide for marketing, but the skin barrier relies on a broader lipid system. Barrier lipids function as a system. Ceramides matter, but they work alongside cholesterol and fatty acids, and delivery structure matters too.
MLE is not only about ingredients. It is about the arrangement. A lamellar delivery system is closer to how the skin barrier is built.
Misconception #3: “More layers means more hydration”
Consumers often layer toner, essence, serum, ampoule, moisturiser, sleeping mask, and oil. If the barrier is leaky, layering becomes repetitive wetting and irritating without fixing the leak.
Hydration only lasts as long as the barrier can retain it. If water escapes through TEWL, the skin alternates between “wet” and “dry”, which can fuel irritation. Barrier-first moisturisers can reduce TEWL more reliably, so fewer steps are needed.
Misconception #4: “Occlusive equals barrier repair”
Petrolatum, thick balms, and heavy butters can reduce TEWL strongly. Some people then assume “this is repairing my barrier”.
However, occlusion is a tool. It reduces water loss, but it does not automatically rebuild the lipid matrix. Some acne-prone patients also feel congested under heavy occlusion. MLE offers barrier support without relying only on heavy occlusion, which can be more comfortable for acne-prone skin. Occlusive products can help temporarily, but barrier repair is about rebuilding the skin’s structure, not just sealing it shut.
Misconception #5: “Natural oils are the same as skin lipids”
Facial oils can make skin feel softer, but they do not reliably replace the skin’s lipid architecture. Some people do well with them, while acne-prone or reactive skin can flare if the oil is too occlusive, oxidises, or comes with fragrance or essential oils. MLE and skin-identical lipid moisturisers are designed for predictability, especially during recovery phases.
Misconception #6: “If it tingles, it is working”
Tingling in barrier-impaired skin often reflects irritation. In a compromised barrier, “active sensation” can be an early sign of inflammation. If your barrier is repaired, skincare should feel neutral, not reactive. MLE moisturisers often play well with sensitised skin because they focus on structure. Skincare that “feels active” is not a requirement for results.
What to look for in a barrier-first moisturiser:
- Fragrance-free and essential-oil-free
- Designed for sensitive or barrier-impaired skin
- Includes skin-identical lipids (ceramides + cholesterol + fatty acids)
- Uses barrier-mimicking delivery (lamellar or MLE-style structure)
- Feels comfortable without stinging or burning
The Koebner Effect and Iatrogenic Damage: Why Treat Acne First Before Anything Else
“Iatrogenic damage” means injury caused by the treatment itself.
When a laser, deep peel, or aggressive procedure is performed on a compromised barrier, the risk profile changes. Trauma on unstable skin can provoke exaggerated inflammation and unpredictable healing.
In certain predisposed individuals, trauma may trigger the Koebner phenomenon, where injury leads to new lesions or flares, such as:
- post-inflammatory hyperpigmentation
- worsening redness
- psoriasis flare-ups
This is why careful clinicians stabilise first. They do not only see “dullness” or “texture.” They see a fragile ecosystem that must be made resilient before it is challenged.
The principle is simple: stabilise the foundation. A strong treatment can be appropriate, but only after the skin is stable enough to heal cleanly.
How long does barrier repair take before lasers?
The real answer is that it depends on each individual. Some people feel improvement within weeks, but stability often requires consistent care and review before proceeding to more intensive procedures.
Dermatology vs. Aesthetics: A Difference of Incentives (Not Just “Philosophy”)
The “Glass Skin” look is not something you buy. It is the visible outcome of a healthy, hydrated, calm barrier.
In aesthetic-led pathways, the plan often starts with a consumer-requested treatment focused on a visible concern.
In dermatology-led pathways, the plan starts with what your skin can safely tolerate and what will improve it in the long term. That difference matters because:
- The dermatologist’s job is to diagnose, not just deliver
- The dermatologist can say no when your skin biology makes a treatment unsafe.
- The dermatologist can sequence care so the “advanced” treatments actually work rather than backfire.
Final Advice: Put Down the Actives
If there is any one piece of advice to take from this article, if you suspect your skin barrier is compromised (e.g., if your skin feels tight after washing, stings when you apply moisturiser, flushes easily, or has a persistent rough texture), please remember the following.
Before you invest in the next trending laser or a stronger skincare routine, invest in your foundation. In acne care, barrier stability is not optional. It is what determines whether your treatments heal or trigger new inflammation.
Key Takeaway
“Glass Skin” is not something you force. It is what calm, well-hydrated, well-sealed skin tends to look like.
A dermatologist’s role is to protect your skin biology from unnecessary harm, and recommend what actually makes sense for your skin first, even if it is not the trending treatment you walked in asking for. Book a consultation with our DermAlly dermatologists for a diagnosis-led plan.
Our articles are written and reviewed by Dr. Coni Liu (MRCS, FAMS) and Dr. Heng Jun Khee (MRCP, FAMS), Ministry of Health-accredited Consultant Dermatologists at DermAlly.
Both are Fellows of the Academy of Medicine (Dermatology) and previously served as Consultants at the National Skin Centre (NSC), bringing extensive experience in medical, surgical, and aesthetic dermatology. They are committed to making expert-led skin education accessible, practical, and clear, helping patients look and feel their best through evidence-based care rooted in science and compassion.